Diabetes Medication Matchmaker
Find Your Best Diabetes Medication
Select your top priorities to see which diabetes medications match your needs best.
Best Match for You
How It Compares to Other Options
Important: This tool is for informational purposes only. Always consult your doctor before making any changes to your diabetes treatment.
For years, people with type 2 diabetes relied on metformin as the go-to pill. But in 2024, a new option entered the scene that’s changing how doctors treat the disease - not just as a blood sugar reducer, but as a tool that can actually help people lose weight, protect their hearts, and even slow kidney damage. The new pill? Oral semaglutide, sold under the brand name Rybelsus.
What makes oral semaglutide different?
Before 2024, semaglutide was only available as an injectable - the same drug behind Ozempic and Wegovy. It worked well, but many people avoided injections due to fear, inconvenience, or needle fatigue. The big breakthrough in 2024 was the FDA’s full approval of a swallowable version. Rybelsus is the first and only oral GLP-1 receptor agonist approved for type 2 diabetes in the U.S. and many other countries.
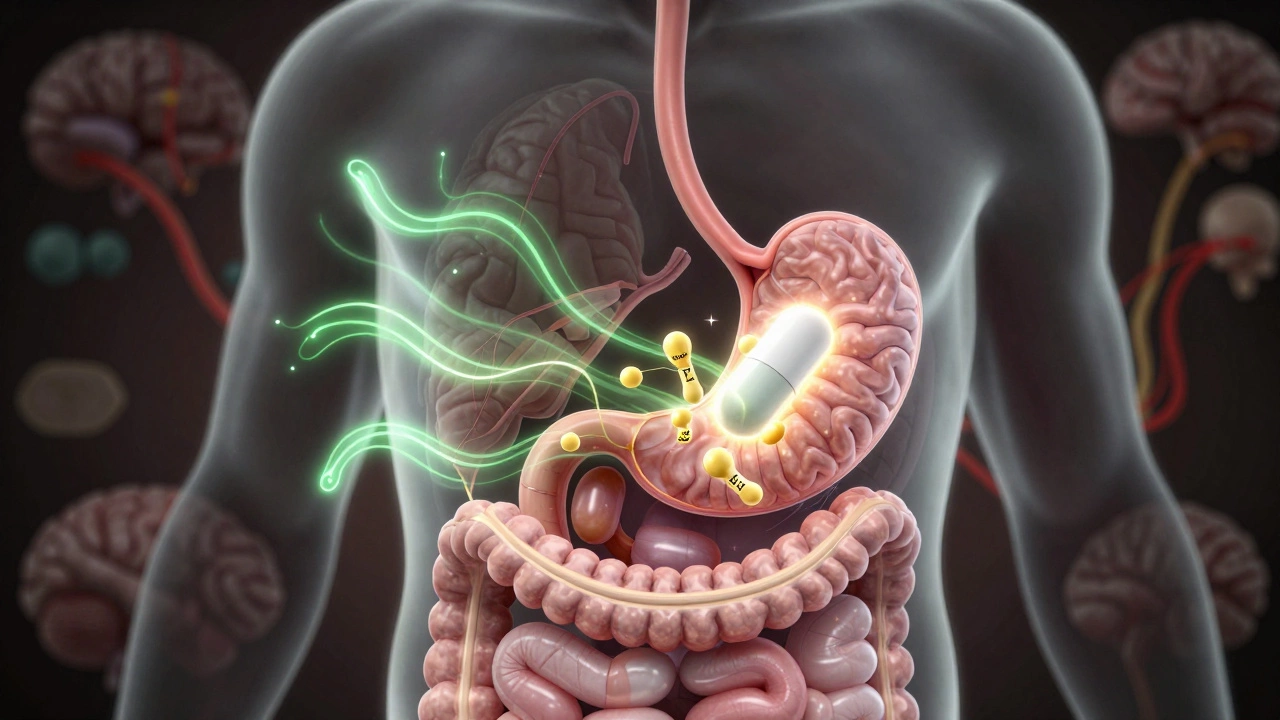
Unlike older pills like metformin or sulfonylureas, which mainly push insulin out or reduce sugar production, oral semaglutide works with your body’s natural hormones. It mimics GLP-1, a hormone your gut releases after eating. This hormone tells your pancreas to make insulin only when blood sugar is high, slows down stomach emptying so you feel full longer, and reduces appetite signals to your brain.
Studies show people taking oral semaglutide lost an average of 5 to 10 pounds over six months - without trying to diet. That’s not just a side effect. It’s part of how the drug works. For someone with type 2 diabetes who’s overweight, losing even 5% of body weight can cut insulin resistance in half.
How does it compare to other diabetes pills?
Here’s how oral semaglutide stacks up against the most common alternatives:
| Medication | How It Works | Weight Loss (Average) | Heart Protection | Side Effects |
|---|---|---|---|---|
| Oral Semaglutide (Rybelsus) | Mimics gut hormone GLP-1 | 5-10 lbs | Yes - reduces risk of heart attack and stroke | Nausea, vomiting, diarrhea (usually mild) |
| Metformin | Reduces liver sugar production | 0-5 lbs | Mild benefit | Stomach upset, bloating |
| SGLT2 Inhibitors (e.g., Jardiance) | Removes sugar through urine | 4-8 lbs | Yes - protects kidneys and heart | Yeast infections, dehydration |
| DPP-4 Inhibitors (e.g., Januvia) | Boosts natural GLP-1 | 0-2 lbs | Neutral | Headache, mild stomach issues |
Notice something? Only two of these - oral semaglutide and SGLT2 inhibitors - have proven heart and kidney benefits beyond lowering blood sugar. That’s not just a bonus. For many patients, it’s the reason doctors choose one over another.
Who benefits most from this new pill?
Oral semaglutide isn’t for everyone. It works best for people who:
- Have type 2 diabetes and are overweight or obese
- Struggle with sticking to injections
- Need help lowering A1C levels (typically above 7.5%)
- Have heart disease or are at high risk for it
- Want to reduce or avoid insulin injections
It’s not recommended for people with type 1 diabetes, a history of thyroid cancer (especially medullary thyroid carcinoma), or multiple endocrine neoplasia syndrome. If you’ve had pancreatitis before, your doctor will think twice before prescribing it.
In India, where nearly 100 million people live with diabetes, the shift toward drugs that treat the whole person - not just glucose numbers - is gaining momentum. Many endocrinologists in Bangalore and Delhi now start with oral semaglutide for patients who fit the profile, especially those with high blood pressure, fatty liver, or sleep apnea.
How do you take it?
Oral semaglutide comes in tablet form, but it’s not as simple as popping a pill with breakfast. The instructions are strict:
- Take it on an empty stomach, first thing in the morning.
- Swallow the tablet whole with a full glass of plain water (at least 4 ounces).
- Wait at least 30 minutes before eating, drinking anything else, or taking other medications.
- Don’t chew, crush, or split the tablet - it’s designed to dissolve in the stomach, not the mouth.
If you forget a dose, skip it. Don’t double up the next day. The tablet is sensitive to food and other drinks. If you take it with coffee, juice, or even a snack, your body won’t absorb it properly. That’s why many people find it easier to take on weekends or days when they’re not rushing.
What are the real-world side effects?
Most people tolerate it well, but nausea is common - especially in the first few weeks. About 1 in 5 people report it, but for most, it fades after a month. Vomiting and diarrhea happen less often. If side effects are too strong, your doctor can lower the dose and slowly increase it over time.
There’s a small risk of gallbladder problems, including gallstones. That’s why people with a history of gallbladder disease should be monitored closely. Rare cases of pancreatitis have been reported, but the risk is lower than with older diabetes drugs like sulfonylureas.
One thing to watch: if you feel unusually tired, dizzy, or confused, it could be low blood sugar - especially if you’re also taking insulin or sulfonylureas. Your doctor may need to adjust those other medications when you start oral semaglutide.
Is it expensive? What’s the cost in India?
Yes, it’s pricey. In the U.S., a month’s supply can cost over $800. In India, the cost is lower but still significant - around ₹10,000 to ₹15,000 per month, depending on the pharmacy and whether it’s imported or locally manufactured. Insurance coverage is limited, and most government schemes don’t cover it yet.
Some private insurers in India are starting to include it in their diabetes management plans, especially for patients with complications. Generic versions are not available yet - the patent protection runs until at least 2030. That means cost remains a barrier for many.
Still, for people who’ve tried metformin and still can’t control their weight or blood sugar, many say the cost is worth it. One patient in Pune told me she dropped from 92 kg to 78 kg in six months. Her A1C fell from 8.9% to 6.4%. She stopped needing insulin. For her, it wasn’t just a pill - it was a new life.

What’s next? Tirzepatide tablets are coming
Oral semaglutide isn’t the end of the story. In late 2024, the FDA approved the first oral version of tirzepatide - a dual GIP/GLP-1 agonist sold as Zepbound and Mounjaro as injections. Early data shows it lowers A1C more than semaglutide and leads to even greater weight loss - up to 15% of body weight in some trials.
The oral version isn’t widely available yet, but clinical trials in India are underway. Experts expect it to hit the market by mid-2025. When it does, it may become the new gold standard - especially for people who need stronger results.
Bottom line: Is it worth trying?
If you have type 2 diabetes and haven’t reached your blood sugar goals with metformin alone - especially if you’re overweight, have high blood pressure, or heart concerns - oral semaglutide is the most significant advancement in diabetes pills since metformin.
It’s not magic. You still need to eat well, move your body, and get enough sleep. But it gives your body a powerful tool to help you do those things more easily.
Ask your doctor if it’s right for you. Don’t assume you’re not a candidate because you’ve been on metformin for years. The goal isn’t just to lower A1C. It’s to live longer, feel better, and avoid dialysis, amputations, or heart attacks. That’s what this pill is really for.
Is oral semaglutide the same as Ozempic?
Yes, the active ingredient is the same - semaglutide. The difference is how it’s delivered. Ozempic is injected once a week. Rybelsus is taken as a daily pill. The pill form is designed to survive stomach acid and be absorbed in the small intestine. They work the same way in the body, but the pill is only approved for type 2 diabetes, while the injection is also used for weight loss.
Can I switch from injection to the pill?
Yes, many people do. Your doctor will usually start you on the lowest dose of the pill (3 mg) even if you were on a higher injection dose. It takes time for your body to adjust. You won’t feel the same effect right away. Most people see full results after 12 to 16 weeks.
Does it cause weight loss in people who aren’t overweight?
It can, but the effect is smaller. People with normal weight typically lose 2 to 4 pounds. The drug works best when your body has more fat to burn and higher insulin resistance. It’s not a weight-loss drug for thin people - it’s a diabetes treatment that happens to help with weight.
How long do I need to take it?
Type 2 diabetes is a lifelong condition. Stopping the pill usually means blood sugar levels will rise again. Most people stay on it indefinitely, especially if it’s helping with weight, heart health, or kidney function. Some doctors may try to reduce the dose after a year if you’ve made big lifestyle changes.
Are there natural alternatives to this pill?
No natural supplement has been proven to match the effectiveness of oral semaglutide. Berberine and cinnamon may help slightly lower blood sugar, but they don’t reduce heart risk or cause significant weight loss. Lifestyle changes - diet, exercise, sleep - are essential, but for many people, they’re not enough on their own. The pill fills the gap where lifestyle alone falls short.
What to do next
If you’re considering this pill, start by getting your A1C tested. Ask your doctor if you have heart disease, kidney issues, or fatty liver - these are key factors in deciding whether oral semaglutide is right for you. Don’t rush into it. Try a 3-month trial with close monitoring. Keep a log of your energy levels, appetite, and blood sugar readings.
For many, this pill isn’t just another medication. It’s the first one that actually makes healthy living easier. And that’s why it’s changing the game in diabetes care - not just in 2024, but for years to come.