Mental Illness Impact Calculator
Assess Mental Illness Impact
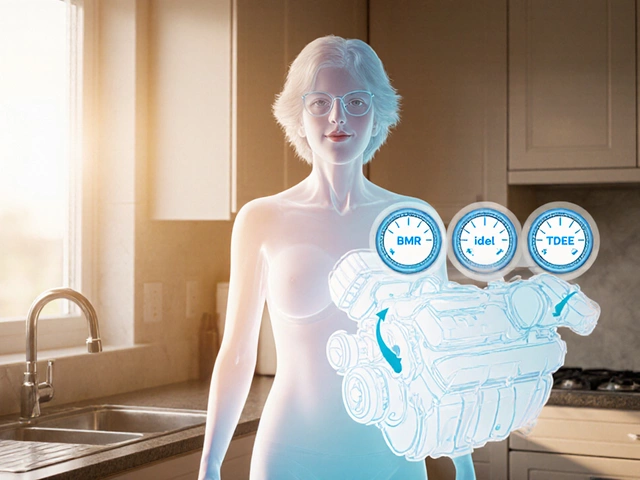
This tool compares the damaging effects of schizophrenia, borderline personality disorder (BPD), and major depressive disorder based on key factors highlighted in the article.
Results
How We Calculated This
We weighted key factors based on the article's findings. Suicide risk carries the heaviest weight (30%) because of its life-threatening nature. Loss of independence (25%), relationship impact (25%), and treatment difficulty (20%) are also critical components of functional damage. Your custom scores help personalize this comparison.
India Resources: Contact The Live Love Laugh Foundation (free helpline) or Vandrevala Foundation for support. In emergencies, call 1800-233-3330.
There’s no single answer to which mental illness is the most damaging-but some come closer than others to destroying lives from the inside out. It’s not about who screams the loudest or who gets the most headlines. It’s about who loses the most: their relationships, their ability to work, their sense of self, and sometimes, their life.
Schizophrenia: The Slow Unraveling
Schizophrenia doesn’t just make someone hear voices. It rewires how they experience reality. People with schizophrenia often lose touch with what’s real-seeing threats where none exist, believing they’re being watched, or thinking their thoughts aren’t their own. The damage isn’t always dramatic. It’s quiet. A college student stops attending class because they’re convinced the professor is broadcasting their thoughts. A father can’t hug his child because he believes the child is an imposter. By the time families realize something’s wrong, years have slipped away.
Half of those diagnosed with schizophrenia never hold a steady job. One in three becomes homeless. The average life expectancy is 15-20 years shorter than the general population-not because of the illness itself, but because of untreated physical health problems, poor nutrition, and high rates of suicide. The brain scans show clear changes: reduced gray matter, weaker connections between regions. It’s not a choice. It’s biology.
Borderline Personality Disorder: The Emotional Firestorm
If schizophrenia quietly dismantles reality, borderline personality disorder (BPD) burns it down in real time. People with BPD feel emotions so intensely that ordinary stress feels like a life-or-death crisis. A breakup isn’t sad-it’s catastrophic. A friend being late isn’t inconvenient-it’s betrayal. This isn’t drama. It’s neurological. Brain imaging shows hyperactivity in the amygdala, the part that controls fear and emotional reactions, and underactivity in the prefrontal cortex, which normally helps us calm down.
The damage? Relationships collapse. Jobs vanish. Self-harm is common. About 10% of people with BPD die by suicide. That’s 50 times higher than the general population. And unlike depression, where people withdraw, BPD often pushes people away-then begs them back. It’s exhausting for everyone involved. Families feel trapped. Therapists burn out. Many go years without proper diagnosis because doctors mistake it for mood swings or attention-seeking.
Major Depressive Disorder: The Silent Killer
Depression doesn’t always look like crying. Sometimes it looks like someone who’s just… gone. They stop answering texts. They skip meals. They sit in the dark for hours. In India, where mental health is still stigmatized, many call it ‘laziness’ or ‘weakness.’ But depression isn’t sadness. It’s a complete shutdown of the brain’s reward system. Dopamine, serotonin, norepinephrine-all out of balance. The person isn’t choosing to be this way. Their brain has stopped signaling that life is worth living.
Over 800,000 people die by suicide each year globally. Depression is the leading cause. In India alone, over 1.3 million people live with severe depression, and fewer than 1 in 10 receive treatment. The cost? Lost productivity, broken families, children growing up without a parent. And because depression hides behind smiles and busy schedules, it’s often the last to be taken seriously-even by the person suffering.

Why These Three Stand Out
Comparing mental illnesses isn’t fair. Each one hurts differently. But if you measure damage by:
- Loss of independence
- Death rate (especially suicide)
- Impact on relationships and work
- Difficulty in treatment
Then schizophrenia, BPD, and major depression rise to the top-not because they’re ‘worse’ than others, but because they attack the core of what makes life livable.
Take bipolar disorder. It’s devastating. So is PTSD. So is OCD. But those conditions often respond better to treatment. Someone with OCD can learn to manage intrusive thoughts. A veteran with PTSD can find relief through EMDR therapy. People with bipolar disorder can stabilize with medication and routine.
With schizophrenia, BPD, and severe depression? Recovery is possible-but it’s harder, slower, and less predictable. Medication helps, but rarely fixes everything. Therapy is essential-but access is limited, especially in rural India. Social support? Often nonexistent. Stigma? Still rampant.
The Hidden Toll on Families
One mother in Bangalore told me her son stopped speaking at 22. He believed the neighbors were poisoning his food. She spent 12 years trying to get him treatment. No one believed her. The hospital said he was ‘just stressed.’ When he finally got diagnosed with schizophrenia, the doctor told her: ‘You’ll need to prepare for the long haul.’ She did. But she never worked again. Her savings are gone. Her other children don’t visit because they’re ashamed.
That’s the hidden cost. Mental illness doesn’t just hurt the person. It ripples through families, jobs, communities. Parents retire early to care for adult children. Siblings drop out of school to help. Marriages break. Children grow up without emotional safety.

What Makes Recovery So Hard?
Access to care is the biggest barrier. In India, there’s fewer than one psychiatrist per 100,000 people. Most rural areas have none. Even in cities, therapy costs ₹1,500-₹3,000 per session. That’s more than a day’s wage for many. Medications are available, but side effects-weight gain, drowsiness, tremors-make people quit. And without consistent support, relapse is common.
There’s also a lack of understanding. Many still believe mental illness is a spiritual issue. Or a character flaw. Or something you can ‘snap out of.’ That myth delays diagnosis by years. By the time someone gets help, the illness has already reshaped their life.
There Is Hope-But It Needs to Be Accessible
Recovery isn’t about curing. It’s about managing. People with schizophrenia can live full lives with the right support. People with BPD can learn to regulate emotions and build stable relationships. People with depression can find meaning again.
But that requires:
- More trained mental health workers, especially in small towns
- Insurance that covers therapy and medication
- Public campaigns that replace stigma with understanding
- Schools and workplaces that recognize early signs
It’s not about choosing the ‘worst’ illness. It’s about recognizing that when someone is drowning in silence, no one should be told to just ‘be strong.’ They need help-before it’s too late.
Is schizophrenia the most dangerous mental illness?
Schizophrenia carries one of the highest risks of early death, suicide, and long-term disability. It often starts in early adulthood and can severely disrupt a person’s ability to work, live independently, or maintain relationships. While not everyone with schizophrenia experiences severe symptoms, without consistent treatment, the long-term damage can be profound.
Can borderline personality disorder be cured?
There’s no ‘cure’ for borderline personality disorder, but many people achieve long-term stability with dialectical behavior therapy (DBT). Studies show that after two years of consistent DBT, up to 75% of patients significantly reduce self-harm and improve relationships. Recovery takes time, but it’s possible.
Why is depression so deadly if it’s common?
Depression is deadly because it often goes unnoticed. People hide it behind smiles, busy schedules, or cultural pressure to ‘stay strong.’ The brain’s reward system shuts down, making even basic tasks feel impossible. Without treatment, the risk of suicide rises sharply. It’s not about being weak-it’s about the brain losing its ability to feel hope.
Are there any mental illnesses worse than these three?
Other illnesses like bipolar disorder, PTSD, and severe OCD can be extremely debilitating. But schizophrenia, BPD, and major depression stand out because they combine high suicide risk, long-term functional decline, and poor access to effective care-especially in places like India. Each one is devastating in its own way, but these three affect the most core aspects of human functioning.
What should I do if I think someone I know has a severe mental illness?
Don’t wait for them to ‘ask for help.’ Gently encourage them to see a doctor or mental health professional. Offer to go with them. In India, NGOs like The Live Love Laugh Foundation and Vandrevala Foundation offer free counseling hotlines. If someone is in immediate danger, contact a local hospital or emergency service. Early intervention saves lives.
Final Thought: It’s Not About Ranking Pain
There’s no medal for who suffers the most. But if we want to reduce the damage, we need to stop minimizing mental illness. We need to treat it like cancer-not something to whisper about, but something to confront with urgency, compassion, and resources.