Weight Loss Estimator
Predict Your Weight Loss
Based on clinical data from the article, estimate your potential weight loss when using Ozempic and/or Metformin with lifestyle changes.
Based on your inputs:
You could expect to lose kg over 12 months.
This represents of your current weight.
People battling type‑2 diabetes often wonder how much weight they can actually shed when their doctor adds Ozempic or metformin - or both - to their regimen. The answer depends on dosage, duration, lifestyle, and individual metabolism, but solid clinical data give us a realistic ballpark.
What is Ozempic and how does it trigger weight loss?
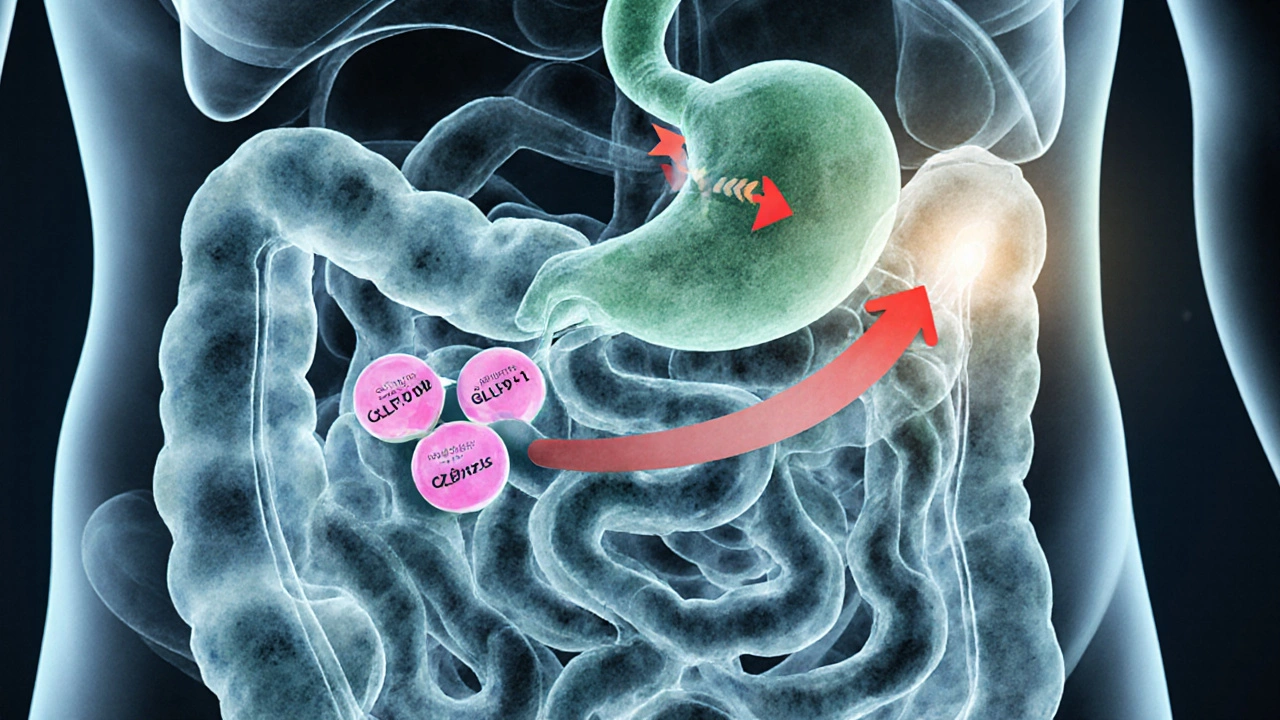
Ozempic is a brand name for semaglutide, a once‑weekly GLP‑1 receptor agonist approved for type‑2 diabetes and chronic weight management. By mimicking the gut hormone GLP‑1, it slows gastric emptying, curbs appetite, and improves insulin sensitivity.
The appetite‑suppressing effect translates into lower daily calorie intake - typically 300‑500kcal less, according to the STEP‑1 trial. Over 68 weeks, participants on 1mg weekly lost an average of 15% of their baseline body weight.
Metformin’s role in weight control
Metformin is an oral biguanide that lowers hepatic glucose production and increases peripheral glucose uptake. While its primary goal is glycaemic control, modest weight loss often follows.
Meta‑analyses of over 30RCTs show a mean reduction of 2‑3kg after 6‑12months of therapy, especially when combined with lifestyle counselling.
Clinical evidence: How much can you realistically lose?
- Ozempic alone: In the SUSTAIN‑7 and STEP‑5 studies, participants on 1mg weekly lost 12‑17% of body weight over a year (≈10‑20kg for a 80‑kg adult).
- Metformin alone: Weight loss averages 2‑3kg in the first 6months, with a plateau thereafter.
- Combination therapy: Real‑world data from US clinics (2022‑2024) indicate an additive effect - patients on both drugs lost about 5‑7kg more than those on metformin alone after 12months.
- Lifestyle only: Structured diet‑exercise programmes typically achieve 5‑10% weight loss (4‑8kg) in the same period.
Putting the numbers together, a typical adult starting at 90kg could expect:
- Ozempic+metformin+diet/exercise: 15‑20kg loss in 12months.
- Ozempic alone+diet/exercise: 10‑15kg loss.
- Metformin alone+diet/exercise: 4‑6kg loss.
Dosage, timing, and safety considerations
Ozempic is started at 0.25mg weekly for four weeks, then titrated to 0.5mg, and potentially 1mg based on response and tolerance. The 1mg dose is where most weight‑loss data sit.
Metformin typically begins at 500mg once daily, escalating to 1,000mg twice daily as tolerated. Gastro‑intestinal upset (nausea, diarrhea) is the most common side‑effect, but it usually subsides within 2‑4weeks.
Both drugs are safe for most adults with eGFR ≥30mL/min/1.73m², but clinicians should monitor renal function, vitaminB12 levels (metformin), and any signs of pancreatitis (Ozempic).
Cost, insurance, and access in 2025
In the United States, a 30‑day supply of Ozempic 1mg costs roughly $900 without insurance, while metformin generic costs $4‑$10. Many insurers cover Ozempic for diabetes but not for weight‑loss indications, though prior‑authorisation rates have risen after the 2023 FDA expansion of the label.
In India, Ozempic is available through specialty pharmacies at about ₹15,000 per month, and metformin is widely accessible for under ₹200 per month.
Maximising results: Lifestyle tips that pair well with medication
- Protein‑first meals: Aim for 20‑30g protein per meal to sustain satiety.
- Fiber boost: 25‑30g daily reduces hunger spikes.
- Mindful eating: Slow down, put utensils down between bites, track hunger on a 1‑10 scale.
- Resistance training: 2‑3 sessions weekly preserve lean mass while losing fat.
- Sleep hygiene: 7‑8hours reduces cortisol‑driven cravings.
When medication‑induced appetite suppression meets these habits, weight loss tends to be more sustained.
Potential pitfalls and how to avoid them
Stopping Ozempic abruptly can lead to rapid regain of appetite and weight within weeks. Always taper under medical supervision.
Metformin’s gastrointestinal side‑effects can be mitigated by taking the dose with meals or using extended‑release formulations.
Both drugs require regular follow‑up labs: A1C every 3‑6months, eGFR annually, and, for Ozempic, a yearly thyroid ultrasound if there’s a personal/family history of medullary thyroid carcinoma.

When medication isn’t enough
If after 6‑12months you haven’t lost at least 5% of body weight, discuss intensifying therapy. Options include:
- Switching to a higher‑dose GLP‑1 agonist (tirzepatide 15mg weekly).
- Adding an SGLT2 inhibitor (empagliflozin) which can contribute an extra 2‑3kg loss.
- Considering bariatric surgery for BMI≥35kg/m² or refractory hyperglycaemia.
These pathways should be evaluated with a multidisciplinary team.
Quick reference checklist
| Parameter | Ozempic (1mg weekly) | Metformin (max 2000mg/day) | Combined |
|---|---|---|---|
| Average % body‑weight loss (12mo) | 12‑17% | 2‑3% | 15‑20% |
| Typical A1C reduction | ‑1.3% to ‑1.6% | ‑0.8% to ‑1.0% | ‑2.0% to ‑2.5% |
| Common side‑effects | Nausea, constipation, possible pancreatitis | Diarrhoea, metallic taste, B12 deficiency | Combined profile; manage individually |
| Typical cost (US, 30days) | $900 (insurance may cover) | $4‑$10 (generic) | ≈$904+$10 |
Bottom line: How much can you lose?
If you stick with the recommended dose of Ozempic weight loss protocol, pair it with metformin and a solid diet‑exercise plan, shedding 15‑20% of your starting weight in a year is very achievable. Even on metformin alone, modest but steady loss of 2‑3kg can improve blood sugar control and lower cardiovascular risk.
Frequently Asked Questions
Can I take Ozempic if I don’t have diabetes?
Yes. Since 2023 the FDA approved semaglutide (Wegovy) for chronic weight management in adults with a BMI≥30kg/m² or ≥27kg/m² with at least one weight‑related condition. However, Ozempic is still prescribed off‑label for weight loss under a doctor’s supervision.
Do I need to stop metformin if I start Ozempic?
No. The two drugs act through different mechanisms and are often used together. Your clinician will monitor kidney function and adjust doses as needed.
How long before I see weight loss?
Most patients notice a reduced appetite within 1‑2weeks. Clinically significant weight loss (≥5% of body weight) typically appears after 3‑4months of consistent treatment.
Are there any long‑term risks with Ozempic?
Long‑term data up to 5years show a low incidence of serious adverse events, but concerns remain about possible thyroid C‑cell tumors (observed in rodents) and pancreatitis. Regular monitoring and proper patient selection mitigate these risks.
What if I don’t lose weight after 6 months?
Re‑evaluate dosage, adherence, and lifestyle factors. Your doctor may consider switching to a higher dose GLP‑1 agonist, adding an SGLT2 inhibitor, or exploring bariatric options if BMI criteria are met.






