Diabetes Medication Assessment Tool
This tool helps determine if newer diabetes medications might be more beneficial than metformin based on your health profile. Results are not medical advice - always consult your doctor before making any medication changes.
Your Results
This is not medical advice. Always consult with your doctor before making any changes to your diabetes treatment plan.
Metformin has been the go-to pill for type 2 diabetes for over 60 years. It’s cheap, safe, and works well for most people. But lately, more and more doctors are turning to other medications - not because metformin failed, but because newer options do more than just lower blood sugar. They protect the heart, help with weight loss, and even reduce the risk of kidney damage. So if you’re wondering what’s replacing metformin, the answer isn’t one drug. It’s a whole new class of treatments - and they’re changing how we manage diabetes today.
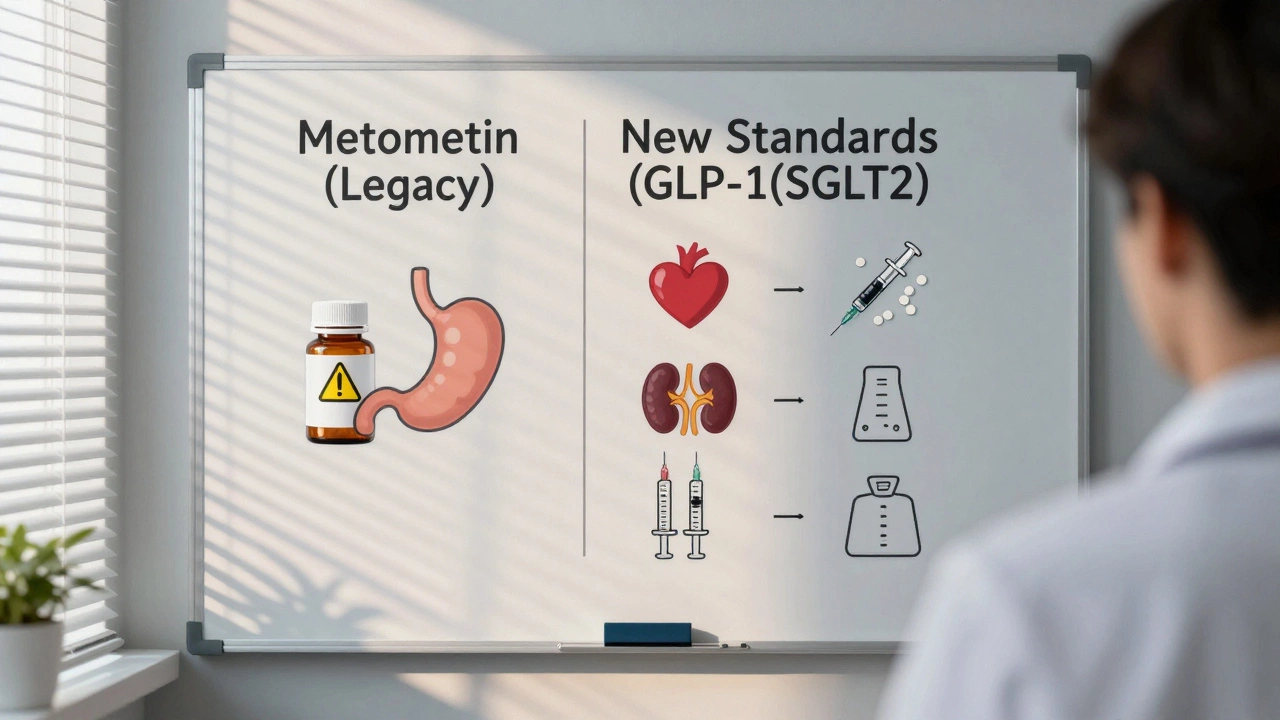
Why metformin isn’t enough anymore
Metformin still works. It lowers liver glucose production and improves insulin sensitivity. But it doesn’t help everyone. About 1 in 5 people can’t take it because of stomach issues. Others don’t lose weight - or even gain it - while on it. And for patients with heart failure or chronic kidney disease, metformin isn’t always the safest choice anymore.
Here’s the real problem: diabetes isn’t just about high blood sugar. It’s about heart attacks, strokes, kidney failure, and early death. Metformin reduces blood sugar, but it doesn’t reliably protect against those bigger risks. That’s where newer drugs come in.
The rise of GLP-1 receptor agonists
Drugs like semaglutide (Wegovy, Ozempic), liraglutide (Victoza), and dulaglutide (Trulicity) are now first-line options for many patients. These aren’t pills - they’re weekly injections. But they do something metformin never could: they trigger weight loss, often 10 to 20 pounds in six months. Some patients lose even more.
Studies show these drugs cut the risk of heart attack and stroke by up to 26% in people with existing heart disease. They also slow kidney damage. In one major trial, patients on semaglutide had 36% fewer kidney events than those on placebo. That’s not just better blood sugar control - that’s life-saving.
Doctors now start these drugs early, especially if a patient has obesity, heart disease, or kidney problems. In 2025, the American Diabetes Association updated its guidelines to recommend GLP-1 agonists as first-choice therapy for many patients - even before metformin.
SGLT2 inhibitors: the other game-changer
Another group of drugs - SGLT2 inhibitors - is also replacing metformin in many cases. These include empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana). They work by making your kidneys flush out extra sugar through urine.
What’s surprising is what else they flush out: extra fluid. That’s why they help with heart failure. In patients with heart failure - even without diabetes - these drugs cut hospitalizations by 30%. They also reduce the risk of kidney failure by 40%.
Unlike metformin, SGLT2 inhibitors cause weight loss, lower blood pressure, and don’t cause low blood sugar when used alone. They’re especially powerful for people who already have heart or kidney disease. In fact, some guidelines now say if you have both diabetes and heart failure, you should start with an SGLT2 inhibitor - not metformin.
When metformin still makes sense
Don’t throw metformin out just yet. For younger, leaner patients with prediabetes or early type 2 diabetes - and no heart or kidney problems - it’s still ideal. It’s affordable. It’s been studied for decades. And it doesn’t cause weight gain.
Many doctors still start with metformin for patients who can tolerate it. But if blood sugar doesn’t drop enough after three months, or if the patient has other health issues, they switch or add one of the newer drugs. That’s the new standard: metformin as a starting point, not the end goal.
What about oral alternatives?
If you don’t want injections, there are newer pills that don’t rely on metformin. One is tirzepatide (Mounjaro), which combines GLP-1 and GIP action. It’s taken as a weekly injection, but there’s an oral version of a similar drug called Rybelsus (semaglutide tablet). It’s the first oral GLP-1 approved in the U.S., and it works just as well as the injection for lowering blood sugar and weight.
Another option is combination pills - like those that mix an SGLT2 inhibitor with a DPP-4 inhibitor (e.g., Janumet XR). But these still don’t match the heart and kidney benefits of standalone GLP-1 or SGLT2 drugs.
Bottom line: if you’re looking for an oral alternative that does more than metformin, Rybelsus is the closest thing. But it’s not cheaper. And it still doesn’t beat the weight loss or heart protection of the injectables.

Cost and access: the real barrier
Here’s the catch: these new drugs cost $800 to $1,200 a month without insurance. Metformin? About $5. That’s why many patients still take metformin - not because it’s better, but because they can’t afford the alternatives.
Insurance coverage is improving. Medicare Part D now covers GLP-1 drugs for diabetes (not just weight loss), and many private insurers follow suit. But prior authorizations are still common. Some patients wait months to get approved.
Generic versions of SGLT2 inhibitors are starting to appear in 2025, bringing prices down. Dapagliflozin is now available as a generic for under $20 a month. That’s making these drugs more accessible - and more likely to replace metformin in routine care.
What does this mean for you?
If you’re on metformin and your blood sugar is under control, no need to rush. But if you’re struggling with weight, high blood pressure, or have heart or kidney issues, talk to your doctor about newer options. Don’t assume metformin is the only choice.
Ask these questions:
- Do I have heart disease, kidney disease, or obesity?
- Am I gaining weight on metformin?
- Have I had side effects like nausea or diarrhea?
- Is my A1C still above 7% after 3 months?
If you answered yes to any of these, you might benefit from a switch. The goal isn’t just to lower your numbers - it’s to live longer, healthier, and with fewer complications.
The future of diabetes treatment
By 2026, metformin won’t disappear. But it won’t be the default anymore. The new standard is personalized care: match the drug to the patient’s biggest risks, not just their blood sugar.
For someone with obesity and early diabetes? Start with a GLP-1 agonist.
For someone with heart failure? Start with an SGLT2 inhibitor.
For someone with no other health problems? Metformin still fits.
This isn’t about replacing one drug with another. It’s about treating diabetes as a whole-body disease - not just a sugar problem.
Is metformin being discontinued?
No, metformin is not being discontinued. It’s still widely used, especially for patients with early type 2 diabetes who don’t have heart, kidney, or weight issues. But it’s no longer the automatic first choice for everyone. Newer drugs are being recommended earlier because they offer better protection against serious complications.
What’s the most effective alternative to metformin?
There’s no single "most effective" alternative - it depends on your health needs. For weight loss and heart protection, semaglutide (Ozempic) is the strongest. For heart failure or kidney protection, dapagliflozin (Farxiga) or empagliflozin (Jardiance) are top choices. The best alternative is the one that matches your specific risks.
Can I switch from metformin to a GLP-1 drug on my own?
No. Never stop or switch diabetes medications without your doctor’s guidance. Stopping metformin suddenly can cause blood sugar spikes. Starting a GLP-1 agonist requires dose titration to avoid nausea and other side effects. Your doctor will help you transition safely.
Do these new drugs cause low blood sugar?
GLP-1 agonists and SGLT2 inhibitors rarely cause low blood sugar when used alone. That’s one of their biggest advantages over older drugs like sulfonylureas or insulin. But if you’re taking them with insulin or sulfonylureas, your risk goes up. Always tell your doctor about all your medications.
Are there any side effects with these new drugs?
Yes. GLP-1 agonists can cause nausea, vomiting, or constipation - especially at first. These usually improve over weeks. SGLT2 inhibitors may increase the risk of yeast infections or rare but serious conditions like Fournier’s gangrene. Both can raise the risk of dehydration. Drinking enough water and reporting unusual symptoms to your doctor is key.
Will insurance cover these new diabetes drugs?
Most insurance plans now cover GLP-1 and SGLT2 drugs for diabetes treatment - not just weight loss - since 2024. But you’ll likely need prior authorization. Generic SGLT2 inhibitors like dapagliflozin are now under $20 a month, making them more affordable. Check with your pharmacy or insurer before starting.






